What is a Nasolacrimal Duct Obstruction?
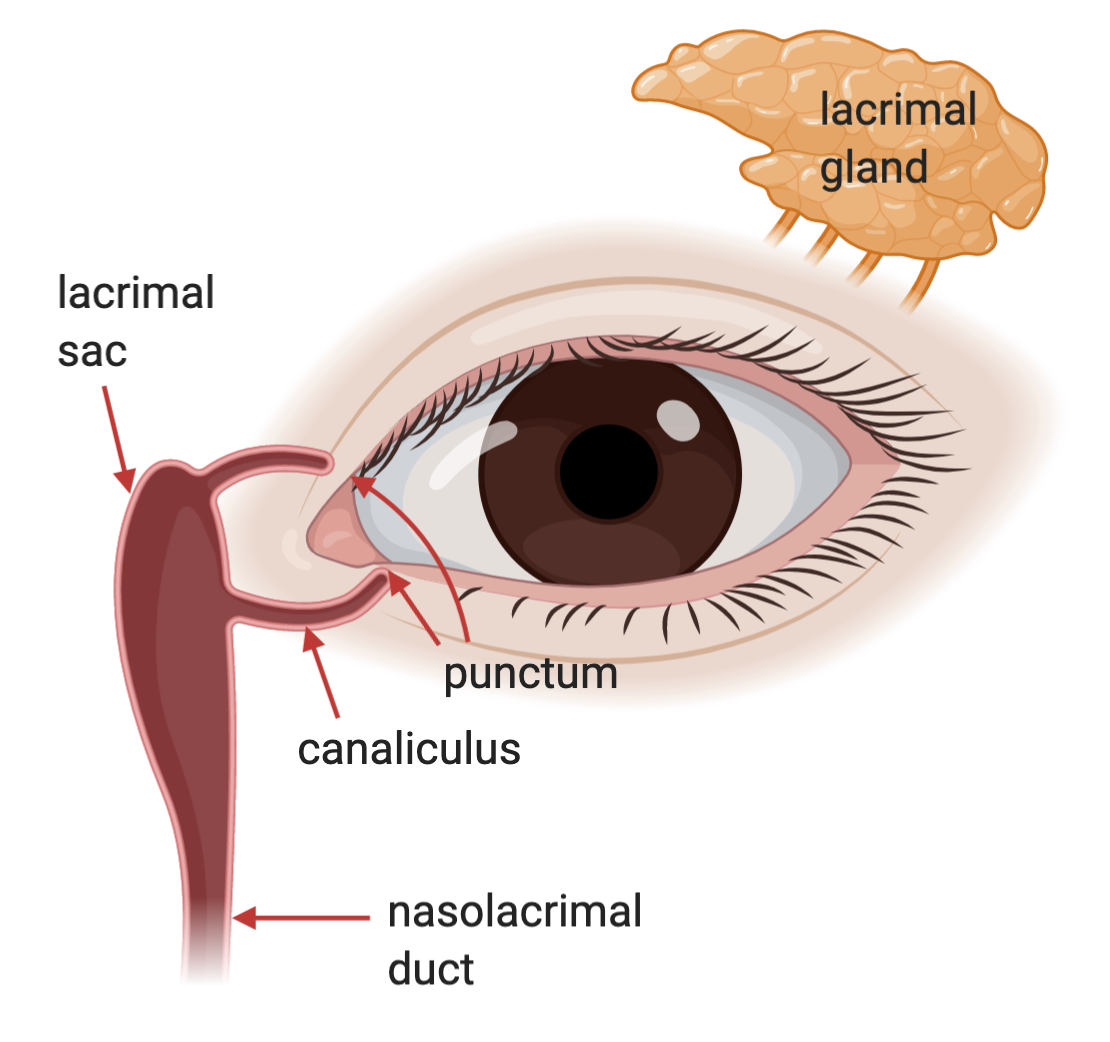
The human tear drainage system begins at the inner corner of the eye and connects to the nose. Tears are produced by the lacrimal gland and normally drain through the nasolacrimal duct, which carries them into the nasal cavity and nasopharynx. This natural drainage mechanism prevents tears from continuously overflowing onto the face
When the tear drainage duct becomes obstructed, patients often experience persistent tearing (epiphora) requiring frequent wiping throughout the day. In more severe cases, or when the duct is completely blocked, bacteria may accumulate and proliferate in the lacrimal sac near the inner corner of the eye, leading to inflammation and infection. This condition, known as dacryocystitis, may present with redness, swelling, and purulent discharge from the inner canthal area, as shown in the image below.

Evaluation of nasolacrimal duct obstruction is commonly performed using an irrigation test. A syringe filled with sterile saline is attached to a small blunt-tipped cannula, which is gently inserted into the punctum at the inner corner of the eyelid before injecting the fluid. If the tear duct is normal, the patient will feel the fluid draining into the nose and throat.
In contrast, if the duct is obstructed, the fluid will not be felt in the throat and will instead reflux onto the ocular surface. In infants and young children, the fluorescein dye disappearance test may be used, where a drop of fluorescein dye is instilled on the eye and observed after five minutes; in a normal tear drainage system the dye nearly disappears, while in cases of obstruction the dye remains more visible compared to the other eye
The causes of nasolacrimal duct obstruction largely depend on age. In newborns and infants, the condition is often due to a persistent membrane blocking the opening of the tear duct into the nose. Treatment may include simple massage over the inner corner of the eye to encourage tear flow and open the membrane. In children older than one year, a fine metal probe can be used to open the obstruction under general anesthesia. For cases requiring further dilation of the tear duct, a lacrimal stent a small silicone tube resembling a thin noodle may be inserted temporarily into the duct and later removed once the passage remains open

In adults, the most common cause of nasolacrimal duct obstruction is narrowing or complete blockage of the duct. When a total obstruction occurs, the standard treatment is surgery to create a new tear drainage passage, a procedure known as dacryocystorhinostomy (DCR). Tear duct surgery in adults is usually performed under general anesthesia and can be approached in two main ways: an external incision near the inner corner of the eyelid, or an endoscopic approach through the nasal cavity without an external scar (though endoscopic procedures may incur additional costs). The success rate of primary DCR surgery is approximately 90–95%
Endoscopic Dacryocystorhinostomy
Currently, the preferred method for treating nasolacrimal duct obstruction is endoscopic surgery through the nasal passage, due to its advantages:
- No external incision or visible scar on the skin
- Does not interfere with the orbicularis oculi muscle, which helps pump tears into the duct
- Faster healing and recovery
- Direct visualization of the nasal structures, allowing identification of additional issues such as nasal septum deviation
For patients with other abnormal symptoms, such as a palpable mass at the lacrimal sac or blood-stained tears, doctors may recommend a CT scan of the nasal cavity before surgery. This helps evaluate whether there is an abnormal mass near the lacrimal sac, as a biopsy may be required instead
Endoscopic surgery through the nose is usually performed under general anesthesia. The procedure involves creating an opening in the bone between the lacrimal sac and the nasal cavity, then connecting the nasal mucosa with the lacrimal sac to allow tears to drain directly into the nasal cavity. During and after surgery, patients may experience some nasal bleeding. The operation typically takes about one hour.
In some cases, the surgeon may place a lacrimal stent or a small silicone tube between the inner corner of the eye and the nasal cavity. This stent is usually removed by pulling it out through the nostril about 1–2 months after surgery. While the stent is in place, patients should avoid pulling it, sneezing, or coughing forcefully, as these actions may cause the stent to dislodge (as shown in the final image).



Pimkwan Jaru-ampornpan, MD



